24-Hour Urine Testing for Kidney Stones

A 24-hour urine collection is a lab test that measures what’s in your urine. It is a timed urine collection used in the metabolic evaluation of urinary stone disease.
The American Urology Association guideline on medical treatment for kidney stone patients recommends 24-hour urine testing for high-risk and/or recurrent stone formers including those with a family history of stone disease, malabsorptive intestinal disease or resection, recurrent urinary tract infections, obesity or medical conditions predisposing to stones (like gout or diabetes). Recurrent stone formers include patients with repeated stone episodes as well as those with multiple stones at initial presentation. Additionally, interested first-time stone formers might be offered metabolic testing to help direct dietary recommendations or potentially initiate medication.
Urine is made up of water and dissolved chemicals, such as sodium, calcium, oxalate and uric acid. The most common stones are made up of calcium and oxalate. Other components that are often measured include urine volume, the concentration of urinary citrate (a major inhibitor of stones), urine pH level, and supersaturation values or calcium oxalate and often uric acid. Think of supersaturation levels as the risk that 2 molecules will join to make a stone, the higher the supersaturation, the higher your risk for forming that particular type of stone. Other analytes include urine potassium, magnesium, phosphorus, ammonium, chloride, sulfate, and nitrogen in the form of urea.
A 24-hour urine collection can be done at your local hospital, but there are also specialty labs like Litholink Co and Mayo Clinic that can also deliver a kit to your home. Discuss the options with your physician.
Here is a sample of what your results may look like:
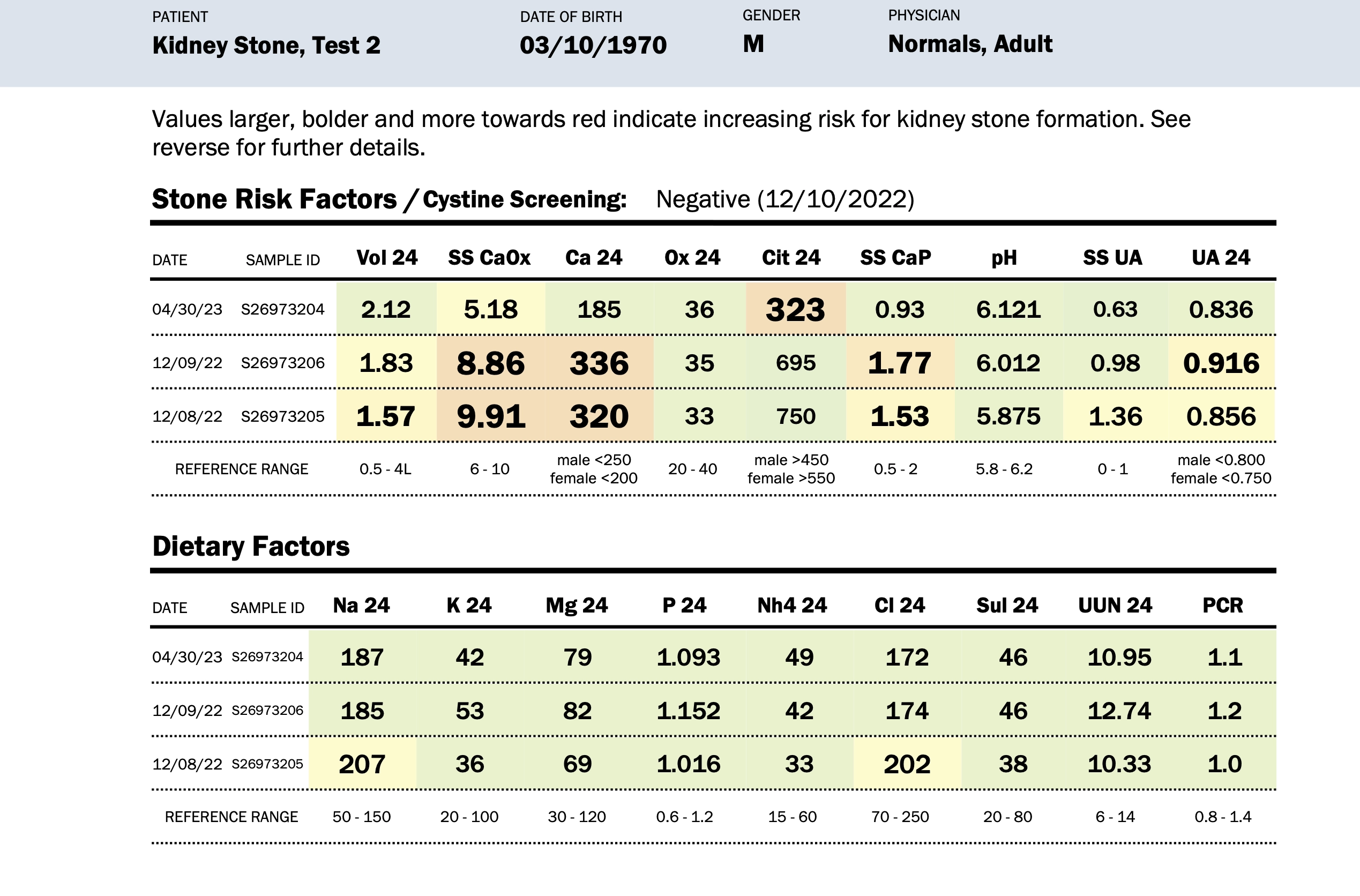
Urine Volume
Decreased urine volume is a major risk factor for stone disease as concentrated urine raises the supersaturation for all stone types. Studies suggest that a goal urinary volume level of 2500 mL per day may be helpful to reduce stone risk. Urine volumes over this amount can decrease stone risk even further.
pH
pH is the measure of how acidic or basic your urine is. Human urine has a pH typically between 4.5 and 8.0. Urine pH is a critical data point as changes in urine pH can increase or decrease the risk of formation for certain stone types. Crystallization of calcium phosphate, calcium oxalate, uric acid, cystine, and struvite are all pH-dependent. Calcium oxalate precipitation is typically not as pH-dependent as the others. Uric acid stone risk is greatest in the acidic range below 5.5. Calcium phosphate crystals form in an alkaline environment of 6.5 and above. Average urine pH over a 24-hour period should fall between 5.7 to 6.3, which limits pH-dependent stone formation.
Sodium
Urinary sodium excretion roughly equates to dietary salt intake. Remember that the primary sources of dietary salt nowadays are from processed foods like bread, chips, soups, sauces, pizza, and take out/fast food. Studies have shown that the more salt you consume, the more calcium ends up in urine, which can increase the risk of forming calcium stones. Lower salt diets typically allow for up to 1500 mg of dietary sodium per day and will likely lower the risk for stone formation.
Magnesium
Magnesium is an inhibitor of urinary crystallization thus decreasing stone risk. Roughly half of the dietary magnesium is excreted in the urine. Low urine magnesium is typically dietary in origin.
Calcium
Elevated urinary calcium concentration can be found in many patients forming calcium stones. Urine calcium concentration is dependent on dietary calcium, sodium intake, and protein intake. We do not typically recommend a low calcium diet! Moderate calcium intake is typically recommended to limit urinary excretion while maintaining bone health. Diets low in calcium can sometimes lead to more calcium and oxalate crystal formation (please refer to our diet section). Modulation of urine calcium is often accomplished with diet changes (reducing salt intake) or medications, depending on etiology.
Citrate
Citrate is a potent inhibitor of calcium crystallization. Low urinary citrate is called hypocitraturia, and this is a common risk factor for stone disease. Hypocitraturia can be from a variety of factors including diet and metabolic diseases. Citrate can be found in foods such as citrus juices, however many of these juices are very high in sugar as well, so it best to be careful and find juices that are low in calories. Citrate intake can also be increased through medications, like potassium citrate. (See our section on treatment of stone disease).
Oxalate
High urine oxalate is another common abnormality in the urine of calcium stone formers. Urinary oxalate comes from both recycling of our own muscle/collagen and from dietary sources. Dietary sources of oxalate include black tea, nuts, chocolate and green leafy vegetables like spinach. Excessive vitamin C supplements are also metabolized to oxalate in the urine. (Please see our diet section for suggestions on dietary control of oxalate). If the 24-hour urine results suggest that high urinary oxalate is a risk factor, lowering dietary intake of oxalate-rich foods may be beneficial.