Dietary Approaches to Preventing Kidney Stones

When dietary habits are thought to contribute to an individual’s risk for kidney stone recurrence, nutrition recommendations to address those habits can be part of the prevention regimen. The converse is also true, i.e., if dietary habits are not thought to contribute to kidney stone recurrence risk, then nutrition recommendations will do little good. In other words, there is no amount of dietary change that can prevent stones that form for a non-dietary reason. But assuming dietary factors are part of an individual’s risk for recurrence, it is important to understand that many variables are considered in formulating a personalized prevention approach. For example:
- People form different types of kidney stones, and not all types are affected by the same dietary factors.
- People have many different risk factors for kidney stones. Even people who form the same types of stones might be forming them for completely different reasons.
- A dietary approach that prevents stone recurrence in one person may not do so another.
- Some individuals follow specific therapeutic nutrition regimens for other diseases or are taking medications that have drug-nutrient interactions. In these scenarios, it makes sense that a nutrition regimen for kidney stone prevention should be integrated according to each person’s unique needs.
In short, there is no “kidney stone diet” that works for all people.
How do you know if your stones are caused by diet? Your individual risk factors for kidney stones should be assessed by your stone prevention team, which might include a urologist, a nephrologist, a dietitian, or an advanced practice provider (such as a nurse practitioner or physician assistant working with your urologist). A urologist is sometimes able to get a stone or fragment during a surgical procedure (or you can save a stone you passed). Laboratory analysis can then identify the stone’s composition, which may help to drive prevention. A urologist or other provider can then place an order to complete a 24-hour urine collection, results of which are critical in identifying why you are forming kidney stones, and also assess for potential underlying factors that may be relevant (such as blood measures or factors within your medical history). Finally, a registered dietitian can diagnose whether certain aspects of your habitual diet are contributing to stone risk, and then “in the context of all the other available information“ determine if your stone risk could be addressed by specific dietary changes.
What dietary factors might be contributing to your stones?
Fluids. Stones are less likely to form in kidneys if urine is dilute. Higher urine output = lower stone recurrence risk. If 24-hour urine output is less than 2 liters, it is advisable to increase fluid intake. A minimum goal is at least 2 liters of urine (about 60 ounces) in a day; even more is better (see image below). This usually requires at least 90-100 ounces of fluids daily, although this varies greatly between individuals. Some people think only water counts. But that’s not true. While low-sugar and low-calorie beverages are preferable, there is room for all types of beverages. If you sweat a lot or tend to have watery stools, you will have to drink even more to produce at least 2 liters of urine. If you forget to drink or don’t have a strong thirst mechanism, then set a timer to remind yourself to drink, or break the day into 3 sections with a goal of drinking at least 30 ounces within each section. Other strategies, such as “smart” water bottles and mobile phone apps, might also be helpful.
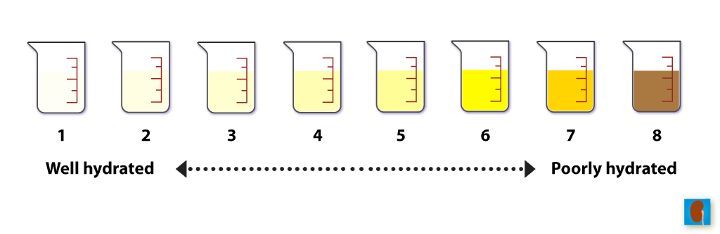
To be well hydrated, urine color should be almost clear, very light yellow, or light yellow (1 through 3). Urine color is a good estimate of hydration for most purposes and it is generally as effective as using volume or urine specific gravity for this purpose. It should be noted that urine color can be altered by certain foods or vitamin intake, both of which can make your urine darker than normal.
- Fruits and vegetables. If the diet is lower for fruits and vegetables, urine citrate might be lower than desired. This increases stone risk because citrate is a potent inhibitor of calcium stones, the most common constituent of most people’s stones. Higher urine citrate prevents calcium stones from forming. If 24-hour urine citrate is low, it is advisable to increase consumption of a variety of fruits and vegetables most every day. This is because all fruits and vegetables have organic acids in them that are converted to bicarbonate in the liver. When this occurs, your kidneys excrete more citrate in urine. Importantly, all fruits and vegetables can help to increase your urine citrate, not only citrus fruits. A good goal is 4-5 most days, such as 2 fruits + 3 vegetables, 3 fruits + 2 vegetables, etc. Another reason to eat more fruits and vegetables is because most provide antioxidants, which could prevent oxidative damage inside the kidneys, which, in turn, may prevent stones. Yet another reason to eat more fruits and vegetables is because they provide “prebiotics”,which are important for maintaining a healthy digestive tract rich in “probiotics”, friendly/good bacteria that work together in multiple ways to prevent different types of stones.
- Calcium. Many people think they should avoid calcium, particularly if they are known or thought to have formed calcium-containing kidney stones. However, avoidance of calcium can actually increase risk for calcium-containing stones not to mention the risk for premature bone loss. The truth is that everyone needs to consume an adequate amount of calcium most every day, i.e., neither too much nor too little. Too much calcium, such as when using supplements, increases risk for calcium stones (both calcium phosphate and calcium oxalate) and vascular calcification. Too little calcium increases risk for calcium oxalate stones in particular. This is because there isn’t enough calcium coursing through the digestive tract to bind with oxalate consumed from certain healthy fruits, vegetables, and whole grains. When calcium and oxalate bind together in the digestive tract, neither is absorbed. This is how an adequate calcium consumption, particularly when timed with meals or whenever plant-based foods are consumed, reduces the amount of oxalate that is absorbed. Less oxalate absorbed = less oxalate in urine. If urine is higher for oxalate, it is advisable to consume calcium-rich foods or beverages with meals. If calcium supplements are required in order to meet calcium needs, a registered dietitian can help to determine how much is needed. It is easy to over-supplement with calcium; and this should be avoided.
- Oxalate. Sometimes diet is not the cause of high urine oxalate. If urine is high for oxalate, a registered dietitian can identify whether it is because of insufficient calcium consumption. In this event, it is advisable to pair calcium-rich foods or beverages with meals. Milk, yogurt, and kefir are good choices. Cheeses and cottage cheese are rich in calcium but also salt, which many are trying to limit. Calcium-fortified plant-based milks or yogurts are good for those who avoid dairy. Calcium-fortified orange juice is another option (best to choose a “diet” or lower-sugar version). While some are warned about eating “too much oxalate,†the elimination of oxalate-rich foods might compromise the nutritional quality of the diet and stone prevention efforts. This is because some of these foods are also those highest for bicarbonate precursors (which supports higher urine citrate), fiber (which contains prebiotics that promote a healthy gut microbiome), antioxidants (which prevent kidney damage), and magnesium, which prevents calcium oxalate stone formation in urine. It is rarely necessary to eliminate or reduce consumption of healthy plant-based foods that contain oxalate, because pairing calcium-rich foods or beverages with meals is usually sufficient.
- Salt. Referring specifically to sodium chloride (also known as “table salt”), higher consumption contributes to higher urinary calcium excretion in susceptible individuals. Higher urine calcium increases risk for calcium-containing kidney stones. While most people think they are adequately avoiding salt if they simply avoid using the salt shaker, nothing could be further from the truth. Only about 10-15% of Americans’ salt consumption is from the salt shaker. Most comes from breads & baked goods, luncheon meats & processed meats, cheeses & foods made with cheese, canned soups & vegetables, salty snacks (e.g., chips, pretzels, popcorn, crackers, salted nuts & seeds), creamy salad dressings, some vegetable juices, frozen entrees, and convenience foods. If urine calcium is high, and if salt consumption is thought to be a contributor (a registered dietitian can help to determine this), then it is advisable to lower salt consumption by avoiding or reducing portion sizes of breads, baked goods, and the other salt-rich foods listed above.
- Vitamin D. Just as with calcium, we need just the right amount of vitamin D — neither too much nor too little. It has become popular in recent years to “mega-dose” with vitamin D. This may contribute to higher urinary calcium excretion. So if urine calcium is high, the amount of vitamin D you take will be examined. If it is too high, you might be asked to temporarily eliminate vitamin D supplements or to reduce the dosage you take.
- Vitamin C. When taken in large supplemental doses (usually >2,000 mg/day), it can raise urine oxalate. This is because the body breaks down the vitamin C it doesn’t need into the smallest molecule possible, which happens to be oxalate. As there is no need for oxalate in the human body, it is simply excreted in urine. Thus, if urine oxalate is high, and if supplemental vitamin C is thought to be a contributor, it is advisable to stop. The amount of vitamin C from 2-3 fruits and vegetables is usually sufficient for most people and does NOT increase risk for too much oxalate in urine.
- Herbal and plant-based supplements. Some contain fairly large doses of oxalate. This is because they are manufactured by taking a large amount of plant material, drying it, and compressing it into tablets or capsules. Most all plants contain some oxalate. So when large amounts are used to make supplements, they can increase oxalate consumption. Examples of supplements known to contain oxalate include turmeric, cinnamon, and green tea extract. Probably most plant-based supplements contain oxalate, but only a few have ever been measured for their oxalate content. If urine oxalate is high, and if herbal or plant supplements are thought to contribute, it is advisable to stop. If urine oxalate is lower in the next 24-hour urine collection, then continued avoidance of the supplement is advisable.
Animal Protein – Kidneystoners.org
Animal protein in meat products increases the risk of stone by increasing calcium, oxalate, and uric acid levels in urine. All three of these changes increase the risk of stones. In studies comparing high meat eaters versus low meat eaters, high meat eaters were found to be at increased risk of forming stones. A randomized study of stone formers restricted to a low meat intake of 52 grams a day (equivalent to 8 oz of beef) in combination with sodium restriction found that the combination reduced stone recurrence by 50% compared to calcium restriction alone (Borghi et al, NEJM 2002).
We recommend that most stone formers try to reduce their meat intake to 6 oz a day. This includes all types of meat: beef, pork, poultry, and seafood.
The USDA recommends a daily allowance of 5-6 oz of protein intake among adults. They also recommend choosing non-meat protein foods such as nuts and beans instead of meat sources. Protein from non-meat sources does not appear to increase the risk of stones.
- A small steak contains about 3-4 oz of protein.
- A quarter pound hamburger with cheese contains 4 oz of protein.
- A chicken breast contains about 5 oz of protein, a chicken thigh about 2.5 oz, a chicken drumstick about 1.5 oz.
- One 5 oz can of tuna contains 5 oz of protein.
- 1 medium egg contains 1 oz of protein.
Lowering your animal protein intake and eating more fruits and vegetables also benefits your overall health by limiting the amount of saturated fats and cholesterol in your diet. This helps to reduce your risk of cardiovascular disease.