Kidney Stone Education Hub
The Kidney Stone Collaborative, along with our partners, developed the resources below for people suffering from kidney stones. Learn more about kidney stones, treatments, interventions, and preventive strategies. Watch videos from our experts, and look through our library of original published work.
Thanks to our resource and content partners WorstPainEver and Kidneystoners.org

Kidney Stone FAQs
6 Basic Dietary Steps to Reduce You Risk for Kidney Stones
To see more in-depth dietary discussion, read the suggestions of Dr. Kristina Penniston
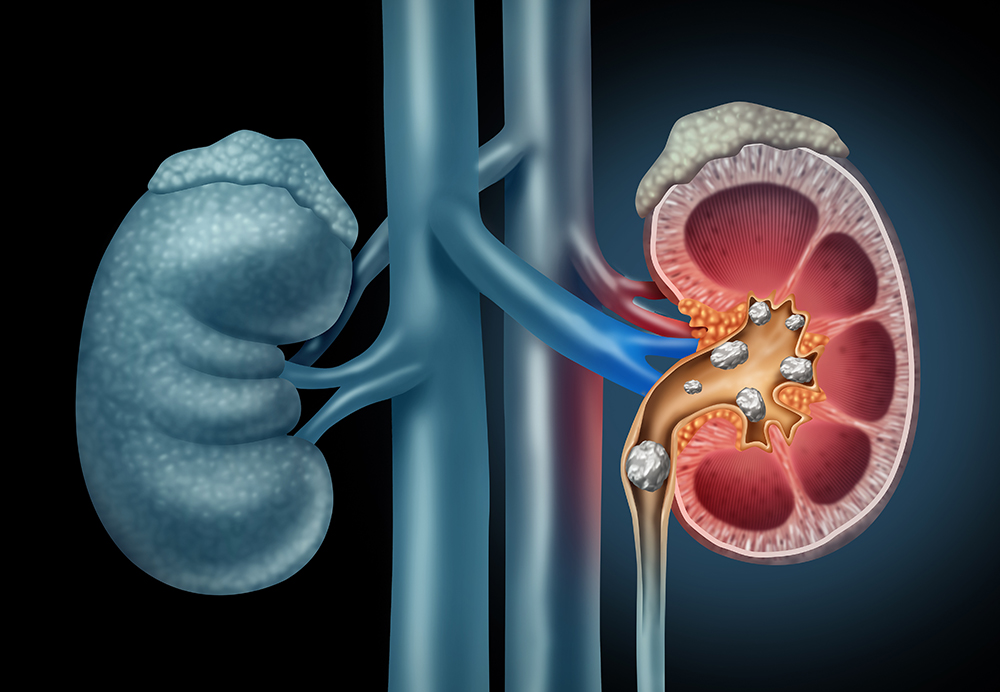
Treatments for Kidney Stones
If you or a loved one have been diagnosed with kidney stones, we understand that you have questions and concerns. One of your main concerns is likely about treatment. Use the following informaton to guide you through treatment options.
Medications for Kidney Stone Prevention
In some patients, the addition of a daily medicine may be recommended by their provider to decrease the risk of future stones. In clinical trials, these medications have been shown to significantly reduce the number of stones events a patient may have.
While many patients are reluctant to take medications and prefer to focus on dietary modification, medications can be a good option, especially in individuals who frequently develop new stones.


Passing a Stone
There are three main factors that your doctor uses to predict your chances of successful stone passage. These include stone size, stone location, and what length of time you have been trying to pass the stone. Many kidney stones will pass spontaneously and will not require surgical treatment.
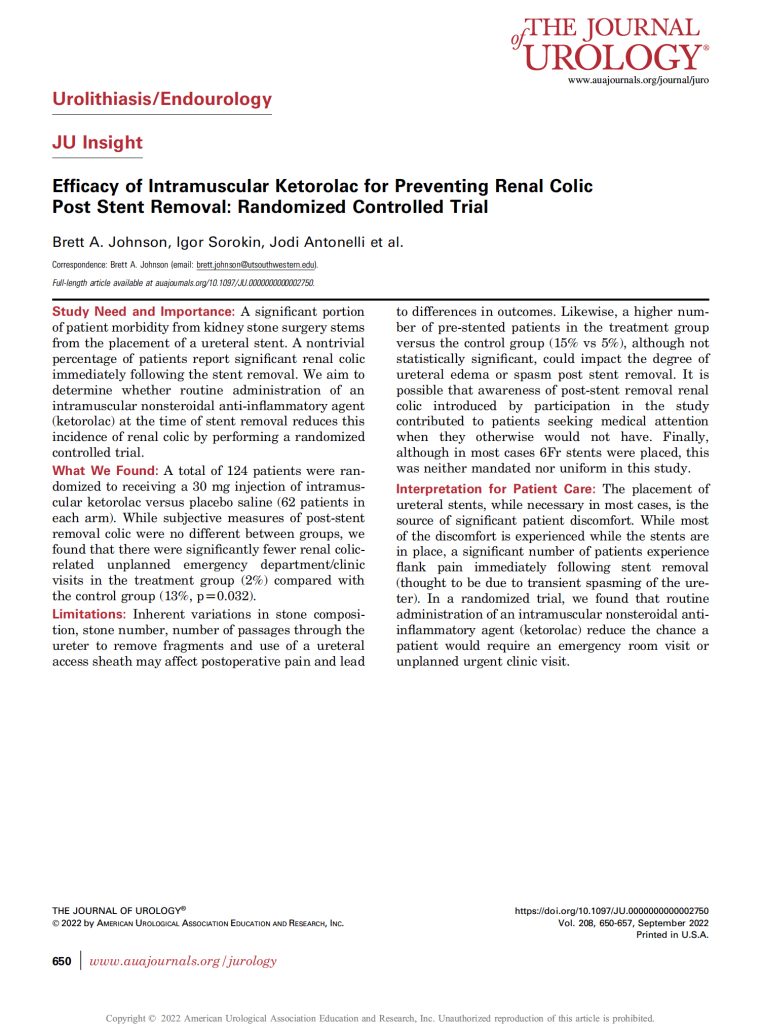
Surgical Options for Removing Kidney Stones
Understanding what is the best option for treating your kidney stone can be difficult. Lear more as we summarize the benefits and drawbacks of each surgical option. While it still won’t make the decision for you, it can help you to make an informed decision when talking to your urologist.

Stay Involved
Nearly 10% of the United States population has suffered from stones. You can help connect with our community and support our mission to accelerate kidney stone research.
Complete the form to learn more about KSC and its initiatives.
By submitting this form, you consent to receive educational emails, research updates, and event invitations from Kidney Stone Collaborative. We will never sell or share your information with third parties. You may unsubscribe at any time.
Information provided is for educational purposes only and is not a substitute for medical advice. Please consult a qualified healthcare professional for personal medical concerns.